50 M with Abdominal distension, shortness of breath since 1 week
This is a case of 50 year old male who is government servant came to the opd with chief complaints of
- Abdominal distension with pain abdomen since 1 week
- Loss of appetite since 1 week
- Shortness of breath since 1 week
- B/L lower limb swelling since 5 days
- Decreased urine output since 5 days
- Reddish yellowish discoloration of urine since 5 days
Patient was apparently asymptomatic one week back then he noticed abdomeninal distention which was diffuse associated with abdominal pain( squeezing type ) not associated with vomotings , loose stools ,fever Aggravated with food intake
Complaints of bilateral pedal edema which is pitting type gradually progressive , extending from ankle to knee joint
C/o decreased urine output and yellowish discolouration of urine since 5 days not associated with fever with chills and burning miturition , frothing of urine
No h/o chest pain , palpitations , excessive sweating .
Complaints of shortness of breath with grade II which is decreased in supine position
No H/o hematemisis , melena
PAST HISTORY
History of dengue 3years ago for which he was hospitalized for 15 days
History of jaundice 2 years ago for which he was transfusions 2 prbc
No similar complaints in the past
no history asthma,epilepsy,thyroid disorders,TB
No history of previous surgeries
FAMILY HISTORY : No significant history
PERSONAL HISTORY
DIET : mixed
APPETITE: Decreased
BOWEL MOVEMENTS: normal
Bladder movements: decreased urine output since 5 days
SLEEP : adequate
Addictions : Alcoholic since 12 years,he used drink 180 ml of whiskey twice a week but from last 6 years he began drinking 180 ml of whiskey daily, but stopped drinking 15 days ago.
DAILY ROUTINE :
He is a government servant ,field worker in revenue department who wakes up at 5 am completes his daily routine and goes to work but most of the times he skips his breakfast . Eats lunch in between 2 - 4 pm because of his busy schedule and goes to bar at 6 pm to drink alcohol daily ( whiskey 180 ml ) and then goes home and eats dinner at 8pm and sleeps by 10 pm.
GENERAL EXAMINATION
Patient was conscious,coherent cooperative
Moderately build and moderately nourished
Pallor : present
Icterus: absent
clubbing: absent
cyanosis: absent
Lymphadenopathy: absent
Edema : absent
VITALS:
On 3/1/23
Temp: afebrile
BP : 110/70 mmHg supine position
Pulse : 92 bpm
RR : 20cpm
Grbs : 101 mg /dl
On 2/1/23
Temp : afebrile
BP : 110/90 mmHg
Pulse : 90 bpm
RR : 22cpm
Spo2 : 98%
SYSTEMIC EXAMINATION
Respiratory system :
On inspection :
Shape of chest is normal
Looks like symmetrically expanding
No scars and sinuses
Trachea is central
On palpation :
no local raise of temperature or tenderness
All inspectory findings were confirmed
On percussion
Purssion note is same on both sides
On auscultation :
Bilateral air entry was present
Crepitus was heard in the right and left inframammary, supra mammary , infra axillary areas
CVS :
S1 S 2 heard apex beat felt at 5 inter coastal space lateral to mid clavicular line no murmors
Per abdomen :
On Inspection :
Abdomen is distended
Visible veins are seen
A rash is seen below the xiphoid process
Umbilicus : flat
Palpation
No local raise of temperature
Abdomen is tense
Percussion - dull note
Bowel sounds -absent
CNS examination
HIGHER MENTAL FUNCTIONS:
Conscious, coherent, cooperative
Appearence and behaviour:
Emotionally stable
Recent,immediate, remote memory intact
Speech: comprehension normal, fluency normal
CRANIAL NERVE:
All cranial nerves functions intact
SENSORY FUNCTIONS
SPINOTHALAMIC TRACT
Pain , temperature ,presure- intact in all limbs
Posterior column:
Fine touch, vibration and proprioception are intact
MOTOR SYSTEM :
Right Left
Bulk:
Inspection. N. N
Palpation. N. N
Tone:
UL. N. N
LL. N. N
REFLEXES
B T S K A P
R + + + + + Flexor
L + + + + + Flexor
CEREBELLUM:
Finger nose In coordination - No
Knee heel in coordination - No
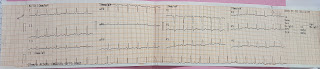
CLINICAL IMAGES
INVESTIGATIONS
Diagnosis: Decompensated liver disease, pancreatitis secondary to alcohol intake.
Treatment
Ascitic tap was done but no fluid was drained
• Fluid restriction less than 1.5 L /day
• Salt restriction less than 2g/day
• Inj Lasix 40mg IV BD
• Syp lactulose 30ml PO
• Maintain 2-3 times passage of stools
• TAB Gabapentin 100mg PO BD
• Inj Monocef
• TAB Aldactone 50 mg PO OD





















Comments
Post a Comment