Sle
A 13 year old female student from suryapet came to the OPD with chief complaints of
Vomitings on Monday night at 10 pm
breathlessness since 1 day
History of present illness:
Patient was apparently asymptomatic before 2020 that is till the age of 11 years,then she noticed swellings in the neck bilaterally,no pain, firm in consistency.
She also had fever which was insidious in onset , intermittent, no night rise of temperature, relieved with medication dolo 3 tid
She also had Non productive cough , no hemoptysis ,relieved with medication.
These symptoms was continued for 2-3 months.
After consulting rmp they started att as her mother has tuberculosis.
Eventually swellings size decreased and symptoms got relieved.
But the fever was not subsiding,so they stopped taking medication.
As rmp suggested , they went to hospital in Hyderabad and got her tested for tuberculosis:
-fnac
-cancer tests
- tb tests
-mantoux
-sputum culture
-cbnaat
because her mother is a known case of tuberculosis.
She got admitted for 10 days and recieved symptomatic treatment
She also had complaints of joint pains wrist and knee.
They suspected it to be automimmune and started her on Hcq and wysolone tab which they used for 15 days.
After that they tested for
ANA ELISA equivocal
ANA IFA negative
ANTI DS DNA ELISA positive
ANTI DS DNA IFA negative
So she went back home
2021
In June she started developing pigmentation/rash over face which then was seen on scalp evident because of hair loss and on trunk since 3 months,not associated with itching.
pedal edema which was upto ankles and progressed till knee in the last 3 months,pitting type.
Then she was taken to area hospital and got tested and the attender(father) was informed that she has tuberculosis.
2022
Ln biopsy was done in May
Mycobacterial gene expert test was done
No reports available
So they started her on ATT and recieved regular treatment for 6months.
2023
Her symptoms settled and she was fine until January 10 when she develop generalized edema.
They went to another hospital and got tested and was told to have proteinuria.
In January and February she had mild fever.
1 week back she developed fever and edema again.
On 13 March that is Monday night 10 pm she had episodes of vomiting 4 episodes ,food as contents,non bilious.
She also developed grade 2 sob and so they got her to here at 5.30am.
In 5th class her weight was 28kgs then in 6th class 23kgs,8th class 21 kgs
After att treatment her weight got improved to 23kgs that is last year
In December 26kgs, 24kgs ,yesterday it was 25kgs.
Past history
K/c/o tuberculosis
Not a known case of diabetes, hypertension, epilepsy, thyroid
Treatment history :
Used ATT for 6 months for TB
Personal history :
Single
Student
Daily routine:
She studied in local school until 4th class.
In 5th class she went to gurukul school and joined in hostel and was fine until 6th class.
In hostel
5 am wake up
Gets ready by 6 am
6:30 am to the ground for yoga,exercises
7 am ragi Java
7.30 am prayer
8am classes
9.15 am breakfast
Classes until 1.30
1.30 to 2.30 lunch
2.30 to 4.30 study hour
4.30 to 5 snacks
5.00 to 6 pm walking ,playing
6 to 6.30 prayer
7 pm dinner
Till 9 pm study hour
9pm sleep
In 7th class she started developing symptoms.
After 7th she stopped going to school as it got worse and she was frequently visiting hospitals.
She went to hostel again after her att treatment and subsidence of symptoms in dec.
Was fine until January and she came back home again .
At home :
6am wake up
7 am tea
Breakfast and fruits
Tablets
Sleeps until afternoon
2.30 to 3 lunch
2 months after taking ATT her appetite was increased and she ate more food, frequently- 5times a day
5pm Walking exercises
Eve 6pm fruits
Songs prayers
8pm dinner
9pm sleep
Personal history:
Diet mixed
Appetite normal
bladder movements oliguria
bowel normal
Sleep decreased
Addictions none
Family history
Mother was diagnosed with TB in 2014 and used ATT irregularly.
Symptoms got worse in 2022 and she died in sept 2022
Birth history:
1st born child
Born in 2010
2nd degree consanguineous marriage
Lscs
Father has no idea about immunisation status
Menstrual history
Not attained menarche yet
General examination:
Patient is conscious coherent and cooperative
Well oriented to time place. And person
Patient examined in well lit room
Pallor present
Icterus absent
Cyanosis absent
Clubbing absent
Lymphadenopathy absent
Edema present
Vitals
On 14/3/23
Bp 130/80mmhg
Pulse rate 110 bpm,regular, normal volume
Respiratory rate 32 cpm
Sp02 99%
On 15/3/23
Bp 130/90 mm hg
Respiratory rate 26cpm
Pulse rate 120bpm
Temperature afebrile
Sp02 98%
On 17/3/23
BP: 130/100 mmhg
PR: 88bpm
RR: 24cpm
TEMP: 97.8
GRBS: 168 mg/dl
systemic examination:
Abdominal examination
Shape - slightly distention.
Umbilicus - Inverted
No visible pulsation,peristalsis, dilated veins and localized swellings.
Palpation
soft, tenderness in right and left Hypochondrium, epigastrium.
Percussion
Fluid thrill and shifting dullness present
Auscultation
Bowel sounds heard
No bruit or venous hum.
Respiratory examination
Bilateral air entry present
Dull note
Vocal resonance decreased
Cvs examination
S1 s2 heard, no murmurs
CNS examination
No focal neurological deficits
Higher mental functions normal
Cranial nerves normal
Sensory examination normal sensations
Motor examination normal
Reflexes normal
Investigations
Spot urine sodium 166mmol/l
Spot urinary potassium 20.5
Abg
pH 7.4
Pc02 14.9 mm hg
P02 79.8mm hg
Hc03 9.2 mmol/l
O2 saturation 96%
Serum electrolytes on 14\3
Sodium 136 meq/l
Potassium 4.4 mEq/l
Chloride 106 meq/l
Serum creatinine 0.6mg/dl
Esr 70 mm
CRP neagtive
Blood urea 29 mg\dl
FBS 100 mg\dl
Blood group 0+
Rheumatoid factor negative
HIV non reactive
Hbs ag non reactive
Urine examination:
Colour pale yellow
Appearance clear
Acidic
Specific gravity 1.010
Albumin ++
No sugar, bile salts, bile pigments, rbc, crystals, casts, amorphous deposits
Pus cells 3 to4 \hpf
Epithelial cells 2 to 3 \hpf
On usg
Liver,gallbladder,pancreas,spleen, uterus,ovaries normal
Moderate ascites
Bilateral pleural effusion
Moderate pericardial effusion
Bilateral grade 2 rpd change
Hb 7.5 g\dl
WBC 4200 cells\cumm
Neutrophils 60
Lymphocytes 36
Eosinophils 02
Monocytes 02
Basophils 0
Pcv 24.6 vol%
Mch 76.4 fl
Mchc 30.5%
Rdw 20.6 %
Rbc count 3.2 million\cumm
Platelet 1.57 laksh\cumm
Smear normocytic normochromic anemia
On 15\3
Serum creatinine 1.0 mg\dl
Sodium 1.37 meq\l
Potassium 4.7
Chloride 104
Spot urine protein 393 mg\dl
Spot urine creat 37.8 mg\dl
Ratio 10.3
Clinical images
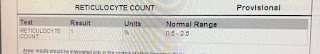
Investigations
Used 4 tablets per day for 6 months regularly.
Provisional diagnosis
?Automimmune disease
Glomerulonephritis secondary to lupus
Treatment
Fluid restriction
Salt restriction
Inj lasix 40mg IV BD
Inj monocef 1gm IV BD
Inj Methyl prednisolone 250mg in 100ml NS IV OD
Tab Aldactone 25mg PO OD
Tab shelcal 500mg PO OD
Vitals monitoring
On 17/3/23
Treatment-
2. SALT RESTRICTION LESS THAN 1.2GM/DAY
3. INJ. LASIX 40 MG IV/BD
4. INJ. MONOCEF 1GM IV/BD(D2)
5. INJ. WYSOLONE 20mg/po/ bd
6. TAB. HCQ/100mg/ PO/OD (5mg/kg)
7. TAB. ALDACTONE 25MG PO/OD
8. INJ. PAN 40MG /IV/OD
9. INJ. ZOFER 4MG/IV/SOS
10. SYP. SUCRALFATE 10ml/PO/OD
11. VITALS MONITORING 2ND HOURLY
12. INFORM SOS
13. GRBS MONITORING 6th HOURLY

























Comments
Post a Comment